We’ve all felt pain and we’ve all felt the relief of its passing. But for people living with chronic pain relief is often brief, if at all.
In broad terms, pain is an unpleasant sensation in your body that makes you want to stop or change your behaviour. In the case of chronic pain, the jabs, throbbing and spasms can persist even after the initial injury heals. In some cases, the cause may not be known. The experience of pain is different for everyone, making it difficult to diagnose and treat.
CHRONIC PAIN: A LIFELONG CONDITION
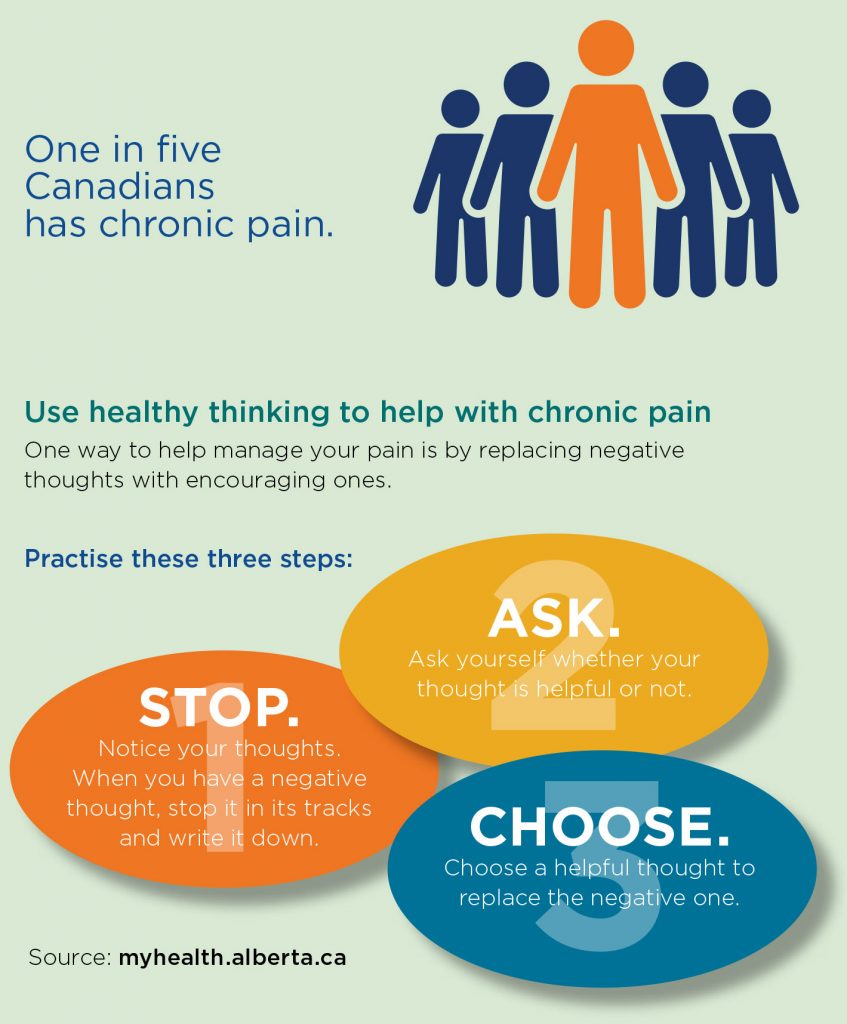
“Chronic pain affects one in five Canadians,” says Dr. June Bergman, medical lead for the extended health team at Calgary Foothills Primary Care Network (PCN). “We now know that it is a disease more of the nervous system than of a specific repairable problem. Chronic pain is a disease and can require lifelong management. This is a different way of thinking. There is not a simple solution or a pill that will fix it.”
To help people living with ongoing pain, Calgary-area PCNs offer pain-management support through a variety of programs and services. They’ve adopted a team approach, drawing on an array of healthcare professionals to tackle different concerns about pain.
More than half of people living with chronic pain have other health concerns such as mental health and digestive issues, obesity and arthritis. “We work with the individual using a biopsychosocial approach that encompasses all the elements that may impact the experience of disease,” Bergman says.
This approach looks at how biological (genetic), psychological (mood, personality, behaviour) and social factors (cultural, socioeconomic, environmental) interact and affect how a disease presents. “We also emphasize the links between sleep, mood, fatigue and function,” Bergman says. “We work with all of these areas to support the patient in being as active as possible and meeting goals for their life.”
SUPPORT ACROSS BOUNDARIES
Primary care doctors at Calgary Foothills PCN can tap into the expertise of other healthcare professionals to help patients with chronic pain through the extended health team. Every team member, whether a pharmacist, kinesiologist, dietitian, nurse, occupational therapist, mental health consultant or social worker, understands what the other team members do. They work together to build on each other’s efforts — and support patients so they can live well with chronic pain.
“Function is a key piece,” says Joe Kwan, manager for Calgary Foothills PCN’s extended health team. “We don’t measure success by whether the pain scale is going down, but rather, has the person been able to move forward in life and engage in society? We want them to be able to live with their disease versus fighting against it. We help them understand that with the right tools, they have the power to get back in the driver’s seat and control their health.”
Christelle Zacharki, a Primary Care pharmacist and the lead at Mosaic PCN’s pain management clinic, agrees. “Outcomes aren’t just about reducing pain, but more importantly, increasing function and quality of life,” she says. “You learn to build resilience and handle pain better.”
Mosaic PCN’s pain clinic also has a team to help patients understand how pain affects their health and daily living. “Our team encourages people to learn skills to manage their pain while co-managing their care with their family physician,” Zacharki says.
“We provide education and active treatment. Moreover, we take a holistic approach. We address the whole person. In fact, the mind-body connection is really crucial.” For example, they show patients how stress can make pain more pronounced and provide solutions to cope better.
MIND OVER MATTER
For Evelyn Kizinkewich, 43, the mind-body connection made all the difference in managing her pain. A patient of the Mosaic pain clinic, she took mental health workshops addressing stress, anxiety and happiness, as well as the Better Choices, Better Health chronic pain course. Now, she has a whole new appreciation for how to cope with osteoarthritis back and knee pain that she’s had for decades.
“A lot of it is the mindset,” she says. “I was a skeptic. But my husband said, ‘If you even take one thing away, that’s good.’ So I went in with an open mind, and I took in so much. Although I’m still in pain, I’m learning to cope and not let it rule me.”
As well, Kizinkewich found staff and other patients helpful. “No one’s ever listened to me before, but the Mosaic PMC’s team makes you feel they understand what you’re going through. And you’re doing it with people who have also been through it. It really helps. You share your stories; it makes you feel better that you’re not alone.”
Another Mosiac PCN patient, Shaleefa Juma, agrees that changing her state of mind helped immensely in dealing with intense pain. Juma developed an antibiotic-resistant strain of rheumatic fever in her 20s, which led to a severe form of Sydenham’s chorea, a neurological disorder that causes involuntary movements. She also has rheumatoid arthritis, an autoimmune disease that affects her joints.
Working with the Mosaic pain clinic helped Juma, now 34, to accept her pain. Her mental health sessions provided the most benefit, despite her not wanting to go at first.
“I was adamant about not going to therapy because it didn’t help me before,” she says. “But it’s been the most helpful thing for me.” Through those sessions, Juma learned that while she can’t change what happened to her, she does have “the will and strength to find a way to have a better quality of life with this disease.”
She adds: “So I finally accepted that I do have a disability, and I have to do things differently. That would have never happened if I didn’t go to the clinic.”
Zacharki says listening can be as important as treatment itself. Because pain is invisible, people may not think that someone is living with it. “We believe patients that the pain is real. That belief can make all the difference,” she says. “We help them focus on how they react to pain. We need to address what’s going on underneath the pain so they can move forward to accept, thrive and have hope.”
MANAGING BEYOND MEDICATION
When Juma first came to the Mosaic pain clinic, she relied on pain medication and wanted to stop using it. “I wanted to have the freedom of my thoughts, and not to sleep all day,” she says. She’s greatly reduced her pain medication with the help of the clinic’s pharmacist, kinesiologist, mental health therapist and doctors.
She still describes her daily pain level as seven on a scale of 10, with 10 being unable to function. “But honestly, it’s not as hard as I thought it would be because now I can go through my life without relying on drugs,” she says. “Everyone who works with me also works together so everyone is on the same page. Before, I’d have to go to at least two appointments a day at different places, and it wasn’t working. Here, I get all my care in one place. And, I feel like everyone here really cares.”
SLOW AND STEADY WINS THE RACE
Kizinkewich’s experience with the Mosaic pain clinic team was equally positive. She met with a nurse, dietitian, kinesiologist and pharmacist. They helped her recognize her stressors, learn relaxation techniques, and most importantly, pace herself. “Before I tried to do everything all at once whenever I felt good and then I’d be down for three days,” she recalls. “Now I know that I can be slow and steady, and I’ll get there. I learned to accept my limitations and work with them, rather than let them get me down.”
She also learned how to manage her medication. “I have a regimen that works all the time so I don’t hoard and run the risk of taking way too many at once like I used to. I don’t have those really bad days anymore.”
Likewise, Ambrosha Pinnock-Kelly can relate to the importance of pacing herself. The 70-year-old had been dealing with pain for 25 years, but recently the pain in her back and legs from her osteoarthritis became unbearable. With the support of the extended health team at the Calgary Foothills PCN, she now effectively manages her pain. “I learned I have to pace myself,” she
says. “So I’m able to sustain myself for a longer time.”
APPLYING WHAT YOU KNOW
The nurses, doctors, pharmacist and physiotherapist all helped Pinnock-Kelly learn coping strategies and put into practice information she’d received over the years, but didn’t know how to apply. “What was different at the clinic was all the support in terms of health advice,” she says. “They actually help you follow through with it. What you already know is reinforced, and somebody encourages you along the way so you can do better and be more consistent. It’s definitely helped me to deal with my pain better.”
Above all, Pinnock-Kelly’s healthcare team gave her the confidence she needed to successfully manage her own health. “The staff checks where you’re at. They see the things that you’re doing right, and they keep encouraging you. That really means a lot.”
The goal of all PCNs’ pain programs is to have patients gain insights into their health and learn to live well despite their pain. It’s not about ending the pain because that’s not always possible.
“At the end of the day, we help the person to have a different perspective in terms of how to manage,” Kwan says. “We point them in the right direction so they can have that ‘aha!’ moment. We
give them tools so they can engage in life, and their family doctor can continue to support them on their new path.”
The coordination of care between pain program staff and family doctors is critical for patients. Kizinkewich’s time with the Mosaic pain clinic greatly improved her relationship with her family doctor, both through her new outlook on life and because now she feels her doctor understands her.
That gives her hope for continued success in managing her pain. “I’m like a whole new person. None of this is a cure for the pain, but it all helps with the mindset, and that helps with the pain. Things are looking up.”
Written by Colleen Seto
This story appears in the latest issue of Health Matters magazine. Read the full issue here.

